The comparison between mechanical and manual ventilation during cardiopulmonary resuscitation (CPR) has been a trending topic in recent research. Many studies have tested if early intubation with transport ventilators improves outcomes over bag-valve ventilation. However, in most of these studies, the quality of conventional manual ventilation was neither controlled nor measured. Consequently, mechanical ventilation was often compared to an uncontrolled and unverified procedure, leading to potentially misleading conclusions.1
The emergence of CPR-specific mechanical ventilation modes
Mechanical transport ventilators are now increasingly available in ambulances. Studies often compare transport ventilators with bag-valve ventilation to find the better method.1 But are we truly comparing what is comparable?
Comparing apples and oranges
Some studies investigating these differences suffer from a major methodological flaw. Indeed, mechanical ventilation or advanced modes are often compared to uncontrolled and unmeasured manual ventilation. 1
On the one hand, mechanical ventilation ensures repeatable performance with controlled parameters such as tidal volume and ventilation rate. On the other hand, manual ventilation during CPR is rarely standardized, meaning patients can easily be hypoventilated or hyperventilated.
In fact, a recent study showed that 60% of patients are hypoventilated during CPR. This hypoventilation correlates with poor outcomes—three times lower survival rates and four times worse neurological outcomes compared to adequately ventilated patients.2
Therefore, in these studies, mechanical ventilation is often being compared to inadequate ventilation—or, in some cases, almost no ventilation at all. This methodological bias makes conclusions unreliable, as no one can be certain that patients in the “manual ventilation” group actually received proper ventilation.
Standardizing manual ventilation with Ventilation Feedback Devices
One solution to address this problem is the use of Ventilation Feedback Devices (VFDs). By continuously monitoring key ventilation parameters such as tidal volume, ventilation rate, and leakage, VFDs provide real-time feedback to rescuers and record objective data on ventilation quality.
These devices help standardize manual ventilation, ensuring it is delivered within recommended guidelines. In doing so, they allow researchers to perform fair comparisons between standardized manual ventilation and mechanical ventilation modes. Only then can we truly evaluate which approach offers the best outcomes for patients in cardiac arrest.

EOlife, the only Ventilation Feedback Device (VFD) to display the volume of gas reaching the patient’s lungs (Tidal Volume).
CE-marked and FDA-cleared medical device enabling real-time measurement of insufflated volume, tidal volume, and ventilation frequency. It provides visual feedback to deliver ventilation following ERC or AHA recommendations.
All mechanical ventilators are not equal
Another important issue with comparative studies on ventilation is the type and quality of transport ventilators that are used.
Indeed, most of the time, the ventilator models selected in such studies are high-end devices (e.g., Hamilton or Medtronic ventilators in (1)). These turbine-based systems offer advanced functionalities that are almost comparable to intensive care unit ventilators. However, these premium devices also come with a high price tag, which makes them unaffordable for many ambulance services.
In reality, most ambulance systems rely on lower-end ventilators, which are predominantly pneumatic. Unlike turbine-based ventilators, pneumatic devices generally lack the ability to deliver a precise tidal volume. This limitation has a direct impact on the quality of ventilation provided during patient resuscitation.
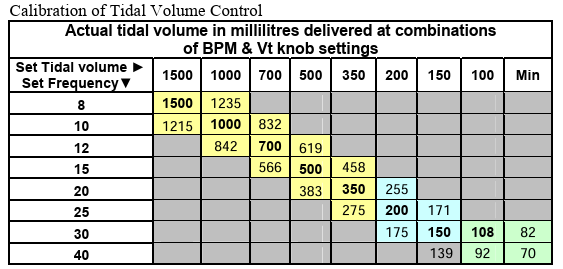
For example, the user manual of a commonly used pneumatic transport ventilator clearly demonstrates the variability in tidal volume delivery depending on the ventilation rate. With a set tidal volume of 500 mL and a ventilation rate of 12 breaths per minute, the actual tidal volume delivered is 619 mL. Such a discrepancy highlights the inability of these devices to ensure accurate ventilation. Moreover, because most of these lower-end ventilators do not provide any real-time feedback on ventilation quality, healthcare providers cannot identify or correct these errors during use.
As a result, high-quality ventilation cannot be consistently achieved, which may have consequences for patient outcomes during CPR
Conclusion
Accurate ventilation during CPR is essential for patient survival and neurological outcomes, yet most comparative studies between mechanical ventilation and bag-valve ventilation fail to control for the quality of manual ventilation. This oversight introduces significant bias and can lead to misleading conclusions about the superiority of one method over the other.
By standardizing manual ventilation with Ventilation Feedback Devices, researchers and clinicians can ensure fair comparisons and improve adherence to international guidelines. Ultimately, the goal is not to favor one technology blindly, but to guarantee optimal ventilation quality.

Are you interested in EOlife to improve your CPR research?
Learn more
References
(1) Min Kim Y, Seok Chai H, Jin Park G, et al. Effect of bag valve ventilation versus mechanical ventilation after endotracheal intubation during cardiopulmonary resuscitation on outcomes following out-of-hospital cardiac arrest: a propensity score analysis. World J Emerg Med. 2025;16(4):313-320. doi:10.5847/wjem.j.1920-8642.2025.062
(2) Idris AH, Aramendi Ecenarro E, Leroux B, et al. Bag-Valve-Mask Ventilation and Survival From Out-of-Hospital Cardiac Arrest: A Multicenter Study. Circulation. 2023;148(23):1847-1856. doi:10.1161/CIRCULATIONAHA.123.065561


