From poor guidelines adherence to improved neurological outcomes
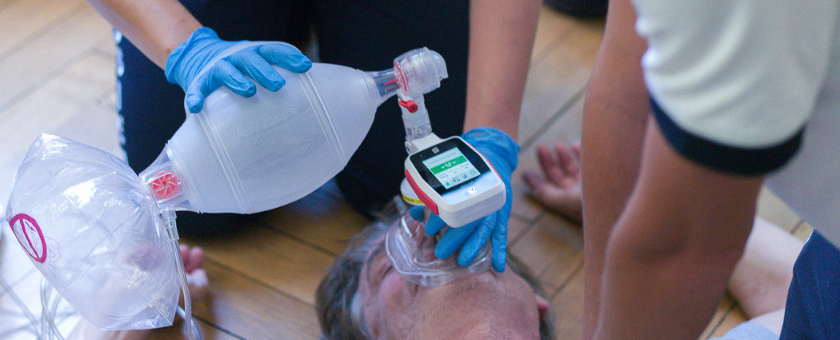
Manual ventilation is a fundamental component of cardiopulmonary resuscitation, yet it remains one of the least objectively monitored interventions during cardiac arrest.
Clinical evidence published throughout 2025 provides a consistent and stepwise evaluation of manual ventilation performance. Ventilation quality without feedback is frequently inadequate. EOlife significantly improves ventilation quality in controlled simulation. Real-world implementation of EOlife is associated with a threefold increase in survival with good neurological outcomes.
Manual ventilation without EOlife: objective evidence of inadequate ventilation
A prospective observational study conducted by the Paris Fire Brigade(1) assessed manual ventilation quality during adult out-of-hospital cardiac arrest using EOlife in blinded mode. This approach enabled objective measurement of ventilation parameters without influencing provider behavior.
Mask leakage: the primary barrier to effective manual ventilation
Despite inclusion of patients managed within a highly experienced Fire & Rescue system, the study demonstrated substantial discrepancies between insufflated and delivered volumes. The results revealed a 41% mask leakage during CPR.
While rescuers insufflated approximately 525–531 mL per breath, delivered tidal volumes were limited to 273–327 mL, indicating that approximately half of each breath was lost, primarily due to mask leakage.
Low guideline adherence despite experienced providers
Only 16.9% of ventilations met recommended tidal volume targets, and nearly 80% of breaths were below 400 mL. The use of a two-person BVM technique resulted in only modest reductions in leakage and did not consistently restore guideline-compliant ventilation.
These findings highlight the intrinsic difficulty of achieving effective manual ventilation during CPR. It demonstrates that in the absence of objective feedback, inadequate ventilation frequently goes unrecognized, even in well-trained emergency medical systems.
Pediatric manual ventilation: simulation evidence supporting real-time feedback
Pediatric ventilation poses additional challenges due to smaller target tidal volumes, higher ventilation rates, and age-dependent variability. A randomized, single-blinded crossover simulation study(2) published in 2025 evaluated manual ventilation performance among EMS clinicians ventilating a high-fidelity pediatric manikin, with and without EOlife X feedback.
EOlife X improves the quality of delivered ventilation
Results show that EOlife X improves both ventilation rate and tidal volume delivery:
- + 60% improvement of tidal volume delivered within the target range. The proportion of breaths with optimal tidal volume increased from 13.5% to 73.3% with EOlife X.
- + 40% improvement of ventilation rate delivered within the target range. The proportion of breaths with good ventilation rate increased from 57% to 96% with EOlife X.
User perception and implications for clinical practice and training
Participants overwhelmingly reported that EOlife X would improve their ability to ventilate pediatric patients appropriately in clinical practice. 99% of participants agreed that a VFD would help them ventilate patients more appropriately.
This study demonstrates that real-time ventilation feedback significantly enhances guideline adherence and technical performance in pediatric ventilation, supporting the role of EOlife as both a training and performance optimization tool
EOlife triples survival with good neurological outcome: real-world outcome data
A retrospective real-world analysis conducted by a Louis-Pasteur University(3) research team evaluated outcomes in out-of-hospital cardiac arrest patients treated by a French firefighter service fully equipped with EOlife.
A threefold higher rate of survival with EOlife
Among 166 OHCA patients, those ventilated with EOlife demonstrated a threefold higher rate of survival with good neurological outcome (CPC 1) compared with patients ventilated without the device (10.4% vs. 3.39%, p = 0.046). Thirty-day survival was also higher in the EOlife group, and all 30-day survivors in this group achieved favorable neurological outcomes. In addition, fewer defibrillation shocks were required among patients ventilated with EOlife.
The principal strength of this study lies in its real-world design, with no predefined research protocol and no modification of clinical practice for study purposes. Although limited by sample size, the statistically significant difference in neurological outcomes indicates a strong association between EOlife use and improved patient-centered outcomes.
Conclusion
The clinical evidence generated in 2025 consistently demonstrates that manual ventilation without objective feedback is unreliable and frequently fails to meet guideline recommendations, even within experienced emergency medical systems. By contrast, EOlife enables accurate, measurable, and reproducible delivery of ventilation in both simulated and real-life resuscitation settings.
Simulation data show that EOlife markedly improves adherence to recommended tidal volumes and ventilation rates, while reducing mask leakage—particularly in high-risk pediatric scenarios where blind ventilation is especially hazardous. Most importantly, real-world outcome data indicate that the use of EOlife during cardiac arrest is associated with a threefold increase in survival with good neurological outcome.
Taken together, these findings strongly support EOlife as a clinically meaningful advancement in resuscitation care. By transforming ventilation from an unmonitored, highly variable maneuver into a controlled and objective intervention, EOlife addresses a critical and long-standing gap in cardiopulmonary resuscitation. Widespread implementation of EOlife has the potential to standardize ventilation quality, improve adherence to international guidelines, and ultimately translate improved ventilation performance into better patient survival and neurological recovery.

Are you interested in EOlife to improve your ventilation quality ?
Learn more
Reference :
[1] Lemoine F, Jost D, Lemoine S, et al. Manual bag-valve-mask ventilation during out-of-hospital cardiopulmonary resuscitation: a prospective observational study. Resuscitation. Published online November 12, 2025. doi:10.1016/j.resuscitation.2025.110895
[2] Finney JD, Siegler J, Wang J, et al. Feasibility and Preliminary Outcomes of a Simulated Prehospital Pediatric Ventilation Scenario Using a Ventilation Feedback Device. Prehosp Emerg Care. Published online September 25, 2025. doi:10.1080/10903127.2025.2558861.
[3] Marie Da Cunha. (2025). Use of a manual ventilation feedback device for the management of out-of-hospital cardiac arrest by firefighters in Doubs_a real-world study. 10.13140/RG.2.2.25073.54884.


